The Psychiatric Hospital Part 5 - Lying to Leave
/I was willing to sacrifice my long-term health for short-term freedom.
Read MoreI was willing to sacrifice my long-term health for short-term freedom.
Read MoreWhile I thought I’d never go into one, I’m certainly glad it was available when I needed it.
Read MoreRecovery after a crisis begins with routine.
Read MoreEven the clothes I wore were searched for contraband or tools I could use to harm myself.
Read MoreIt took my fourth hospitalization before I realized the folly of lying to expedite my release.

During my first three hospitalizations, I learned the rules and then acted accordingly. Doctors, nurses, and other caretakers are, in my experience, personally invested in a person getting well. I had many wonderful interactions with compassionate and empathetic professionals at each hospital where I spent time. That said, the medical business is a business.
Insurance companies are not keen on paying for beds for patients who are stable. A hospital cannot be financially sound if patients are kept on the ward until their caretakers are absolutely sure a patient is capable of taking care of themselves, or at the very least, not in any danger of self-harm.
It is a system that constantly cycles people in and out. Because it is a system, though, it can be gamed.
I am exceptionally good at putting on a facade to the world. In my first hospitalizations, I lied.

Told the nurses I felt great. I smiled. I held doors open for other patients. I politely requested shaving privileges, and did my very best to be of no concern to those running the ward. This strategy worked brilliantly to get me released because there was no behavior the doctors or nurses could point to where I demonstrated the desire for self-harm.
I appeared psychologically “stable,” and that meant I should be released, and my bed given to someone at more acute risk of overdose, self-harm, etc.
I knew the system. I had read about emergency psychiatric hospitals and insane asylums. The best patient is typically one that causes no problems. So I lied and became the best patient I could at the expense of my health.
At this point someone might rightly condemn me: “How could you lie to your doctor? Didn’t you want to get better?” Spare me.
If everyone told their doctor the truth, there would be no medical drama category on Netflix.
I wanted out of the hospital, and I was willing to sacrifice my long-term health for short-term freedom.
There are no quick fixes for mental illness, and lying can only be maintained for so long. Eventually, I did not have the energy to keep the facade going. My mask of normality crumbled away.
My last hospitalization was a result being committed following my outburst in the seclusion room. I stayed in my bed for days. A nurse kept coming into my room to encourage me to venture out and interact, but I stubbornly stayed under my sheet. After a while, though, it was pretty boring by myself, and I shuffled outside.
Six years after my first hospitalization I had finally had it with putting on a show of normality. It was exhausting and counter-productive. Once I stopped playacting and started working on my recovery, life got better.
It is realistic to expect that I will be back in a psychiatric hospital someday in the future. I learned that fact from a delightful older woman who checked herself into the hospital every year or so for a couple of weeks. She knew that when she did not feel safe, she should be in the safest place possible.
That was a great lesson to learn. I can use the hospital just like any other treatment. That understanding makes it much more bearable to willingly be locked into a ward, watch Law & Order SVU reruns, eat poor food, and talk with doctors.
Using the system, as opposed to gaming the system, was the lesson I wish I knew years and years ago.
My seclusion room story requires a bit of set up.
I voluntarily committed myself to Ridgeview in 2011, and was given a brief tour to get comfortable with my new little world. Part of that world was a seclusion room.

It’s pretty bare, but safe.
It consisted of four walls with a solid, rubber mattress on the floor. Why solid rubber? So that someone could not strangle themselves with sewn fibers.
A brilliant white light radiated from the light fixture that was mounted flush with the ceiling. Why flush? So that someone could not hang themselves from it.
A substantial, but easily opened door with a large window separated this little psych ward from the big psych ward. Why the window? So the nurses could keep an eye on the patient. The door was strategically located directly across from the nurse’s station for even easier tracking.
There is no straight jacket, no one is getting chained to the wall, and no one is locked in without round-the-clock supervision. But, I distinctly remember thinking,
“I’ll never be in one of those.”
Life, as I have come to learn, loves irony.
In the fall of 2016, I had the “choice” between involuntary commitment or voluntary commitment at a facility in Maryland. More on that in a later post.
After my release, I entered an Intensive Outpatient Program, or IOP. Basically, you go to the hospital every morning, stay till three, and get to sleep in your own bed at night. This program gradually gets a person into a more regular routine, and they can more easily transition into the life they choose to live.

Bedlam from 'A Rake's Progress' 1733, By William Hogarth - “Bedlam” was the byname of Bethlem Royal Hospital due to the noise. Visitors were welcome! For a shilling or two, you could walk through the hospital and gawk at the crazy people.
I was there for extreme panic attacks, that were a side effect of a new medication I was cycled onto by my psychiatrist. I have never experienced such terror, and I hope to never experience anything close to the sensations I had while on that medication. I write this because it explains why I needed the seclusion room on a crisp Friday afternoon in November.
“They’re looking at me.”
“They’re spying on me.”
“They’re judging me.”
Such are the thoughts of a paranoid mind in the early stages of a panic attack. Truth be told, the nursing students had no idea who I was, and they certainly had no evil intentions toward me. But, my mind was unaccustomed to seeing them. The unexpected and unwanted presence of several new faces in my safe hospital ward triggered a massive panic attack.
Almost entirely paralyzed by fear, I somehow got a nurse’s attention and communicated with him by grunting and shaking my head “yes” or “no” to his questions. He gave me a high strength, anti-anxiety medication, which was nice, but at that point, it was about as effective as putting a single sandbag in the path of a massive flood. Using our meager method of communication, we agreed that I wanted to go into the seclusion room to feel safe and ride out the worst of the panic attack, but I could not move.
Four nurses picked me up in my chair and placed me in the room. They lifted me out of the chair, removed my clothes and put a paper gown on me. Why paper? Think about it and you’ll realize why.
A nurse asked if she would be safe sitting in the room with me. I grunted, “yes,” but my mind was on fire, and after a few minutes I told her:
“I need you to get out of this room and lock the door.”
She did, and I lost it.
Dramatic recreation
You already know that seclusion rooms are designed to prevent someone from significantly hurting themselves. I knew this too. So I used the room to cause pain that I could control.
I punched the walls. I chained combinations together until my knuckles bled. I screamed. I paced. I raged. When I could no longer lift my hands, I slammed my head against the wall.
I did not feel agony. I WAS agony.
I unleashed all of my panicked energy while the nurses and doctors pleaded for me to stop. Protocol dictated that they stay outside the room. Sure, it would have been nice to have someone restrain me, but the safer course is to let a person burn themselves out until they are no longer a threat to themselves or their caretakers.
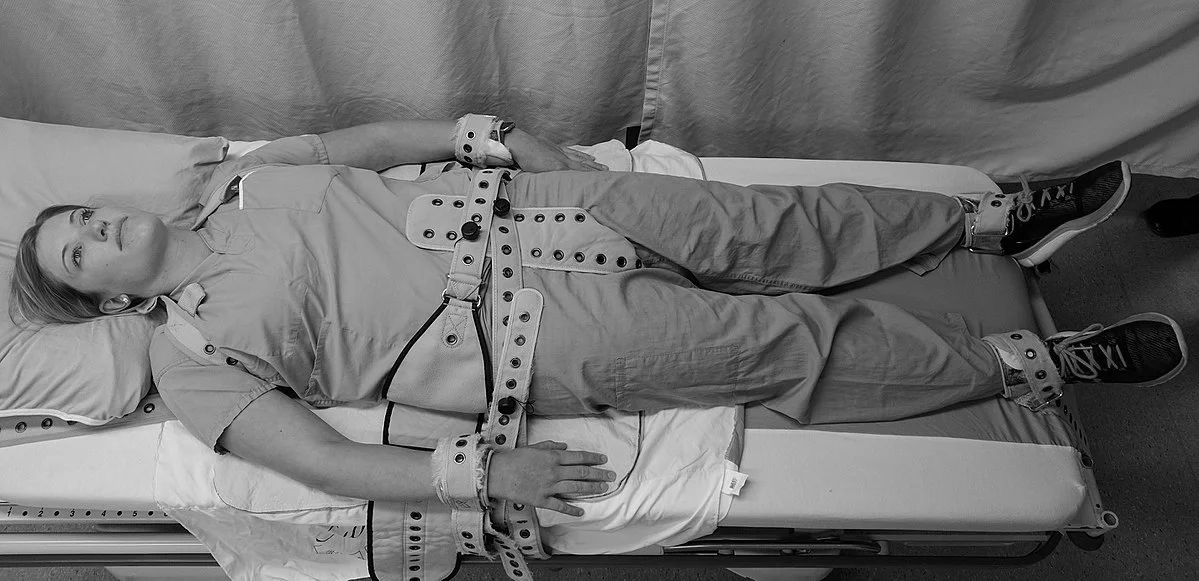
Most hospital protocols specify that restraints be used for the least amount of time necessary.
Eventually, everything slowed down. I collapsed onto the mattress and the door opened up. Several large men secured my limbs and put me on a gurney, to which my wrists and ankles were strapped.
Didn’t I write no restraints earlier? They are used as a final resort to protect a person who has clearly demonstrated the recent capacity to hurt themselves, and to protect those around them.
A nurse injected me with Haldol, an antipsychotic drug that “decreases excitement of the brain.” It’s the human equivalent of horse tranquilizer - you get real chill, real quick. Then she gave me another injection to counteract the side effects of Haldol.
I woke up two days later with a pounding headache and swollen knuckles, and all I could think of was how wrong I was so many years ago.
Routine.
Visit any psychiatric ward, anywhere in the country, and you will find a daily routine that the caretakers follow. Why is routine important? Why are vitals taken each morning? Why are meals served at the exact same times? Why are groups part of every day?
Because in the throes of withdrawal or with someone not long after a suicide attempt - the mind is shattered.

USS Constellation - I run by it most mornings.
Imagine your mind as a ship. You are the captain of the ship, but you are also every officer, every deckhand, and even every piece of wood and rope that make up the ship. Then a storm comes, the ship/you runs aground, and splinters into pieces. You reach out and grab hold of a floating plank, where you desperately try to keep your head above water in the heaving seas.
You become the captain of a wood plank, floating alone in the chaotic abyss.
Routine is the starting process for rebuilding a ship. You don’t throw wood and nails into a dry dock and expect a ship to come together without a plan. Nor should you expect that to happen with your mind.
Most hospitals follow a routine:

Vitals are taken every day so the nursing staff and doctors can notice any significant changes in a person’s physical health.
Morning
Wake up, vitals, meds
Breakfast
Group session
Afternoon
Lunch
Group session
Break
Evening
Group session
Dinner
Meds
The routine is dull, uninteresting, and unexciting - by design!
Imagine you’re desperately gripping your wooden plank, and, by some miracle, a party cruise liner breaks over the horizon. You are rescued and immediately thrown into a world of bright lights, loud noises, curious food, and you haven’t a clue what the destination is. You’re grateful to be out of the water, certainly, but you have a whole new host of issues to navigate.

Now imagine you are saved by the Coast Guard. Everyone is wearing the same uniform, everyone fits into a particular role, everyone is calm in the face of danger. A medic checks you out, you’re given a blanket and a cup of coco, and told where you will be taken to next. You’re just as grateful to be out of the water as you were in the first scenario, but all of your issues are taken care of for you.
That is the magic of routine. It gives a mind in chaos something to hold onto. Something that makes sense. Something that can be counted on.
That is where recovery can begin.
A GIGANTIC thank you to the following people for breaking my $1,000 goal for the Baltimore Out of the Darkness Walk!
Collette Dixon
Roger and Margo Coleman
Lou and Mary Jo Corsetti
Caitlin Corsetti
James Hunt
Samantha Perrine
The Smith Family
Natalie Wills
Kate and Mark Bernal
Andi O’Connor
The Assaf Family
Kevin Greene
The Arney Family
Jim Fiora
Cara Morris
There is a common misconception that a psychiatric hospital will be eerily similar to “One Flew Over The Cuckoo’s Nest". Uncompromising doctors treating crazy patients with a strong helping of electroshock therapy and powerful antipsychotic medication. Such were my preconceptions of what was an underwhelming, boring, but ultimately helpful experience.

On July 5th, 2011 I voluntarily checked myself into the Ridgeview Institute after my hanging attempt. At intake I answered a myriad of medical and personal history questions in triplicate, was interviewed about my most recent mental health problems, given an ID wristband, and led behind the first of many locked doors in the complex.
An orderly brought me into Cottage C, which specialized in addiction recovery and mental health issues consisting of depression, bipolar disorder, and schizophrenia. From intake I was sat down, got my blood pressure and temperature taken, then told to wait for a staff member to search me and inventory my belongings.
After thirty minutes of people watching, which is very amusing on a psychiatric ward, a nurse ushered me into a very utilitarian office where all of my belongings were searched. Even the clothes I wore were searched for contraband or possible weapons or tools I could use to harm myself.
After the search I was fed a rather delicious meal of fried fish and vegetables, and then a nurse showed me to my bedroom where I met my roommate. A very polite older gentleman there for treatment of his severe alcoholism. Once I saw the bed, I laid down and tried to rest because I had not slept well since my suicide attempt three nights earlier.

I was on a fifteen minute bed check, which meant that every quarter of an hour a nurse came into my room with her smartphone as a flashlight to check that I was still breathing.
You may think that is a little much, but it is essential for someone not far removed from a suicide attempt. The bed checks also establish a regular pattern for a shattered mind to recognize and accept.
My mind was in utter chaos, and knowing a nurse would check in on me every fifteen minutes was oddly comforting.
Life on the 7th Shelf is my way of sharing how a person can live well with depression, anxiety, and suicidal ideation.
The 7th Shelf was written by Dante in The Inferno, as the Wood of the Suicides.
For me, living on the 7th shelf is challenging but I have found my means for winning the daily battle against the worst my mind can throw at me.
We aim to create a space of hope, filled with resources, information, tools, and more for mental health awareness and suicide prevention. We’re committed to Gordon’s vision of sharing different methods of thinking to help those with and without mental illness live more fulfilling lives.
Contact us
corsetti007@me.com

Call or text 988 for the Suicide & Crisis Lifeline for help. In an emergency, please call 911.
If you or someone you know is seeking help for mental health concerns, visit the National Alliance on Mental Health (NAMI) website, or call 1-800-950-NAMI(6264).
For confidential treatment referrals, visit the Substance Abuse and Mental Health Services Administration (SAMHSA) website, or call the National Helpline at 1-800-662-HELP(4357).