Life in a Psychiatric Hospital - Part 5 of 5
/It took my fourth hospitalization before I realized the folly of lying to expedite my release.
During my first three hospitalizations, I learned the rules and then acted accordingly. Doctors, nurses, and other caretakers are, in my experience, personally invested in a person getting well. I had many wonderful interactions with compassionate and empathetic professionals at each hospital where I spent time. That said, the medical business is a business.
Insurance companies are not keen on paying for beds for patients who are stable. A hospital cannot be financially sound if patients are kept on the ward until their caretakers are absolutely sure a patient is capable of taking care of themselves, or at the very least, not in any danger of self-harm.
It is a system that constantly cycles people in and out. Because it is a system, though, it can be gamed.
I am exceptionally good at putting on a facade to the world. In my first hospitalizations, I lied.
Told the nurses I felt great. I smiled. I held doors open for other patients. I politely requested shaving privileges, and did my very best to be of no concern to those running the ward. This strategy worked brilliantly to get me released because there was no behavior the doctors or nurses could point to where I demonstrated the desire for self-harm.
I appeared psychologically “stable,” and that meant I should be released, and my bed given to someone at more acute risk of overdose, self-harm, etc.
I knew the system. I had read about emergency psychiatric hospitals and insane asylums. The best patient is typically one that causes no problems. So I lied and became the best patient I could at the expense of my health.
At this point someone might rightly condemn me: “How could you lie to your doctor? Didn’t you want to get better?” Spare me.
If everyone told their doctor the truth, there would be no medical drama category on Netflix.
I wanted out of the hospital, and I was willing to sacrifice my long-term health for short-term freedom.
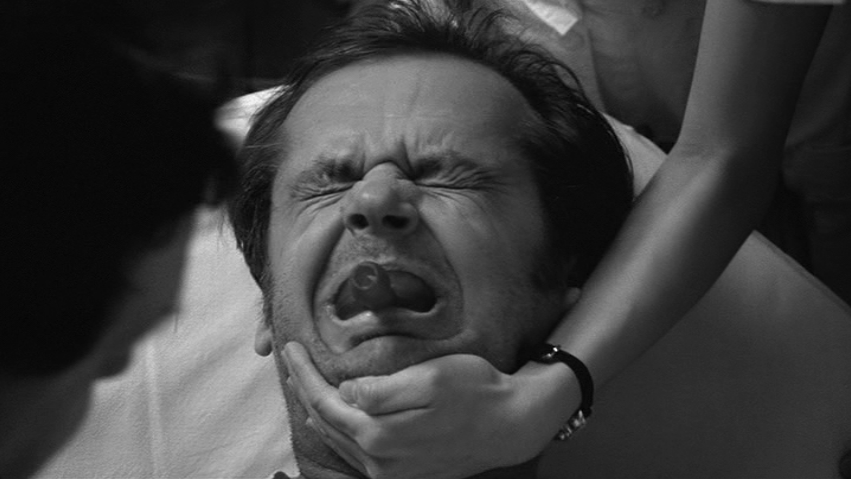
There are no quick fixes for mental illness, and lying can only be maintained for so long. Eventually, I did not have the energy to keep the facade going. My mask of normality crumbled away.
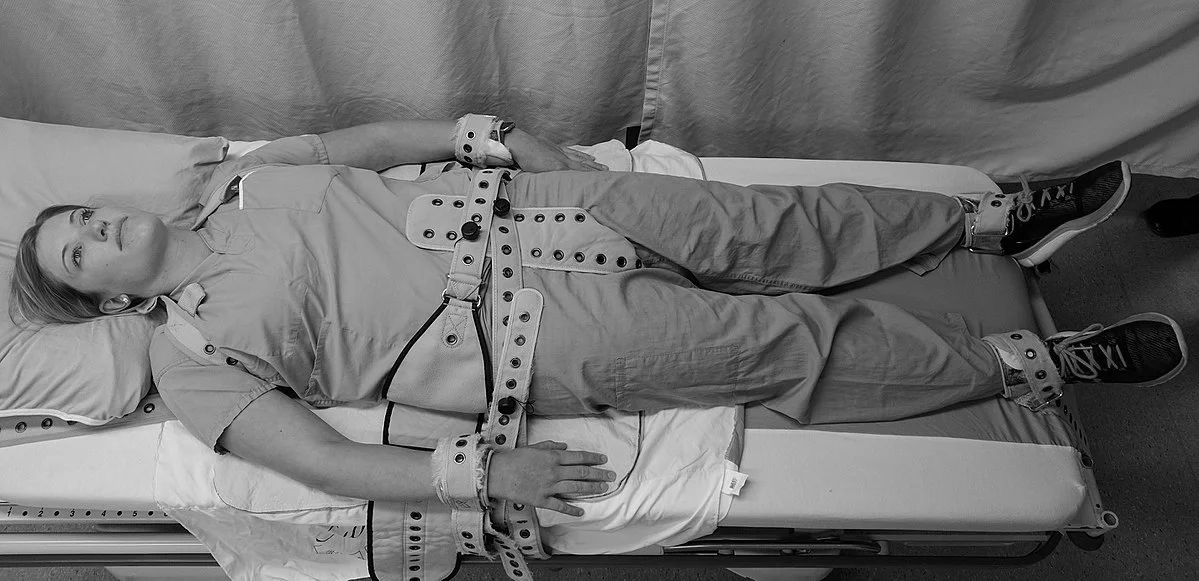
My last hospitalization was a result being committed following my outburst in the seclusion room. I stayed in my bed for days. A nurse kept coming into my room to encourage me to venture out and interact, but I stubbornly stayed under my sheet. After a while, though, it was pretty boring by myself, and I shuffled outside.
Six years after my first hospitalization I had finally had it with putting on a show of normality. It was exhausting and counter-productive. Once I stopped playacting and started working on my recovery, life got better.
It is realistic to expect that I will be back in a psychiatric hospital someday in the future. I learned that fact from a delightful older woman who checked herself into the hospital every year or so for a couple of weeks. She knew that when she did not feel safe, she should be in the safest place possible.
That was a great lesson to learn. I can use the hospital just like any other treatment. That understanding makes it much more bearable to willingly be locked into a ward, watch Law & Order SVU reruns, eat poor food, and talk with doctors.
Using the system, as opposed to gaming the system, was the lesson I wish I knew years and years ago.